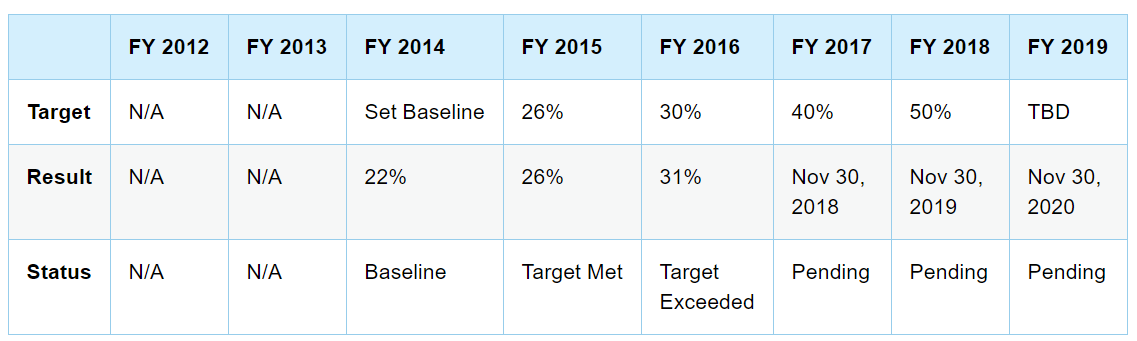
A primary objective of value-based care is to increase provider accountability in delivering better health outcomes. This is driven out through Alternative Payment Models (APMs) such as capitation, gainsharing, and bundled payment arrangements. As a provider, one of the key factors of participation in any one of these models is taking on a bigger share of the risk. As costs continue to soar, CMS and other payers continue to invest in these types of arrangements. In fact, CMS was pushing to have at least 50% of all payments made to a provider, tied to some type of APM by 2018.
The need to understand risk
While there is a significant amount of weight behind these initiatives, there is also considerable pushback from the healthcare community. What we hear and see with providers participating in these value based arrangements is that (1) many of them don’t even know what APM’s their participating in (2) They don’t know which patients they’re responsible for, month to month (3) They’re concerned about the risk, when the infrastructure to determine that risk isn’t in place or isn’t robust enough to address influencers that have a huge impact on patient behavior, and ultimately their performance profile.
There is widespread evidence out there that supports physicians’ arguments and substantiates their concerns that risk modeling, in its current state does not go far enough to perform an apples-to-apples comparison of performance. These types of studies prove that there are strong relationships between socioeconomic status (SES) and adverse health behaviors (such as smoking, physical inactivity, less nutritious diets, and excessive alcohol consumption), and between SES and biological risk factors (such as high blood pressure, high serum cholesterol and fibrinogen, and obesity; Davey Smith et al., 1996a,b; Kaplan and Keil, 1993; Lynch et al., 1997a; Marmot et al., 1991).
Risk adjustment today
Most risk adjustment models out there today, look at basic factors, such as age, sex, and location. Some go as far as to look at conditions and prescription usage. Only a few commercial solutions actually look at other contributing factors like frailty, lab markers, ED and inpatient utilization. Even then, some think that these don’t go far enough to explain the determinants of health.
Risk adjustment of the future
To really get to an apples-to-apples comparison, we need to consider social and psychological conditions, a.k.a. sociopsychological factors. These sociopsychological factors include, but are not limited to socioeconomic status; social support and networks; occupational stress, unemployment, and retirement; social cohesion and social capital, and religious beliefs.
Today, risk adjustment is used pretty broadly in APM’s, in areas such as: (1) determining financial benchmarks, like per member per month or case rate amounts; (2) establishing payment penalties placed on providers that don’t meet financial targets; (3)setting standards for quality measures such as readmissions, ED utilization, and mortality rates. As the demand for APM adoption continues to grow, and risk adjustment continues to play such a significant role in reimbursement under these models, it will be imperative to get granular with risk modeling. That is, if we want to engage physicians at the level we need them to be, in order for value-based healthcare to succeed in delivering better outcomes.